NODDI - 4D Flow
Background
While Alzheimer’s disease (AD) is typically considered to be a disease of gray matter, white matter (WM) alterations are also known to occur and may even precede gray matter degeneration, suggesting that WM damage may not just be a secondary process to damage of gray matter. Large scale WM alterations can often be visualized on diagnostic images as white matter hyperintensities, which have been shown to be strong predictors of AD and dementia. While there have been a number of studies assessing macroscopic WM alterations in AD cohorts, there have been only a handful of studies assessing alterations at the level of the tissue microstructure. It has been hypothesized that microstructural WM degeneration is, to some extent, the result of microvascular injury. According to the two-hit hypothesis presented by Berislav Zlokovic, cardiovascular and cerebrovascular disruptions damage the brain’s microcirculation, leading to adverse structural changes. This hypothesis is further supported from recent findings that indicate that blood brain barrier dysfunction, hypoperfusion, altered cerebrovascular hemodynamics, and various cardiovascular risk factors are associated with AD progression and may even precede amyloid deposition. It is thus plausible that vascular disease and amyloid deposition are synergistically involved in Alzheimer’s disease.
I would suggest the wonderful textbook published in 2020: Vascular Disease, Alzheimer’s Disease, and Mild Cognitive Impairment: Advancing an Integrated Approach which posits that Alzheimer’s disease, vascular disease, and mild cognitive impairment should be viewed as a continuum disease, as opposed to distinct disease processes.
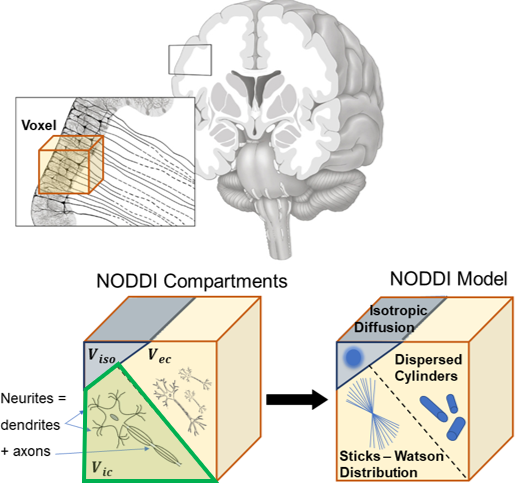
In this study, we combine diffusion tensor imaging (DTI) and 4D flow MRI to measure white matter microstructure and intracranial hemodynamics. Specifically, we use neurite orientation dispersion and density imaging (NODDI) using multi-shell DTI data in order to analyze neurite density index (NDI), a surrogate measure for WM axonal density.
Additionally, pulsatility index, carotid pulse wave velocity, and total cerebral blood flow were also measured. In our initial study, this was performed in 20 AD subjects and 41 cognitively normal (CN) age-matched individuals. However, future studies look to apply this to 136 subjects with PET imaging.
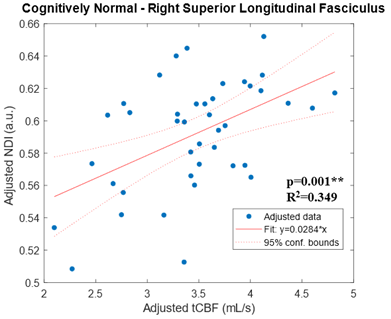
Using tract-based spatial statistics (TBSS) and a pre-labelled WM atlas, we showed that there were significant WM microstrctural differences in many tracts between cognitively normal and AD subjects (which has been shown in several other studies). More interesting, we used linear regression (adjusted for age and sex)) to show that altered WM microstructure was associated with lower total cerebral blood flow in normal individuals. However, this relationship was not shown in individuals with AD. Additionally, there were no correlations with vascular pulsatility or vessel stiffness and white matter microstructure.
Collaborations:
Andrew Alexander Lab, Doug Dean III Lab
Abstracts
Oral Presentation
- Roberts, G. S., Rivera-Rivera, L. A., Johnson, K. M., Johnson, S. C., Dean III, D. C., Alexander, A. L., Wieben, O., & Eisenmenger, L. B. Assessment of Cerebrovascular Disease and White Matter Neurite Density in Alzheimer’s Disease. 2021 ISMRM & SMRT Annual Meeting & Exhibition; 2021 May 15; Vancouver, BC, Canada.
Manuscripts
In-Preparation
- Spahic, A., Roberts, G. S., Peret, A., Rivera-Rivera, L. A., Moody, J. F., Dean III, D. C., Alexander, A. L., Johnson, K. M., Johnson, S. C., Wieben, O., & Eisenmenger, L. B. Assessment of Cerebrovascular Disease and White Matter Neurite Density in Alzheimer’s Disease. To Submit to Journal of Alzheimer’s Disease.

Leave a Comment
Your email address will not be published. Required fields are marked *